Vaginismus is a medical condition that affects many women, often causing confusion, frustration, and emotional distress. Despite its prevalence, vaginismus is a topic that is often under-discussed and misunderstood. In this blog post, we’ll dive deep into what vaginismus is, its causes, symptoms, and the various treatment options available to manage and overcome it.
What is Vaginismus?
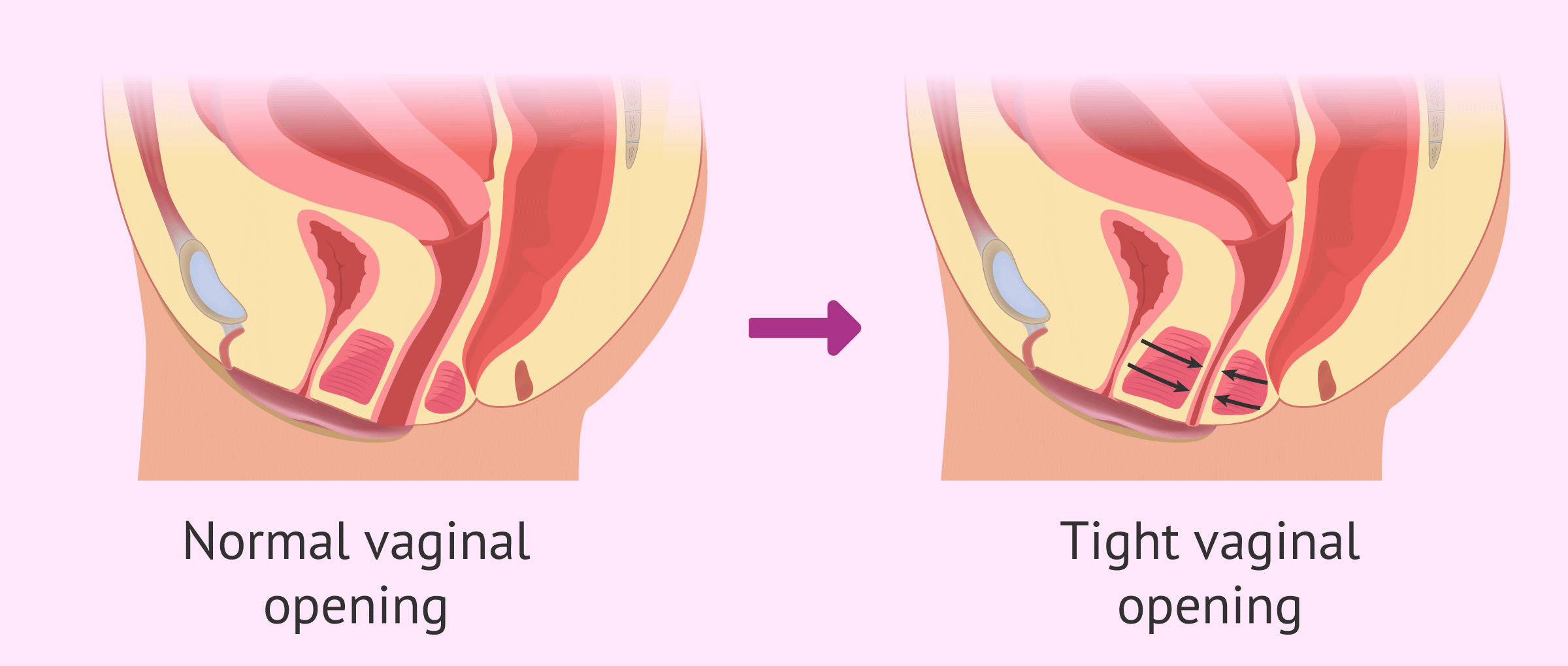
Vaginismus is a condition where the muscles of the vagina involuntarily tighten or spasm, making penetration—whether during intercourse, gynecological exams, or the use of tampons—painful or impossible. It’s important to note that vaginismus isn’t a psychological disorder per se; rather, it is a physical condition that is often influenced by psychological factors.
There are two types of vaginismus:
- Primary Vaginismus: This is when the condition is present from the first experience with vaginal penetration, such as during the first attempt at intercourse or a gynecological exam.
- Secondary Vaginismus: This occurs after a period of normal sexual activity or vaginal penetration. It may develop due to various reasons such as trauma, an infection, childbirth, or other medical conditions.
Causes of Vaginismus
The causes of vaginismus are varied and can be both physical and psychological. Often, it’s a combination of factors that lead to the development of this condition. Some common causes include:
1. Psychological Factors
- Trauma or Abuse: A history of sexual abuse, rape, or trauma can lead to a fear of penetration, causing the pelvic muscles to tighten involuntarily.
- Anxiety and Stress: Fear of pain or fear of intimacy can create muscle tension, leading to vaginismus. Anxiety about sexual performance, body image, or past negative experiences can also play a role.
- Cultural or Religious Beliefs: In some cultures or families, there may be strong beliefs about sexuality that can make sexual activity seem shameful or intimidating. These beliefs can contribute to fear and anxiety about intercourse.
2. Physical Factors
- Infections or Medical Conditions: Chronic vaginal infections, pelvic inflammatory disease (PID), or vaginal dryness due to menopause or breastfeeding can lead to painful intercourse and may trigger vaginismus.
- Childbirth and Pelvic Surgery: Women who have experienced trauma during childbirth or pelvic surgery might develop vaginismus due to the physical changes in their pelvic muscles or lingering pain.
- Pelvic Floor Dysfunction: An imbalance in the pelvic floor muscles—either tightness or weakness—can contribute to the spasms that occur in vaginismus.
Symptoms of Vaginismus
The main symptom of vaginismus is the inability to have vaginal penetration due to the involuntary contraction of the vaginal muscles. This can result in a variety of experiences, including:
- Painful Intercourse (Dyspareunia): Pain during sex is a common symptom, and this can range from mild discomfort to severe pain.
- Difficulty with Gynecological Exams: A woman with vaginismus may find it difficult or impossible to undergo a pelvic exam or have a Pap smear, which can make visits to the doctor challenging.
- Fear or Anxiety Around Sexual Activity: The anticipation of pain or the fear of penetration can lead to emotional distress, causing avoidance of sexual intimacy altogether.
- Inability to Use Tampons: Some women with vaginismus may find it painful or impossible to insert tampons due to the muscle spasms in the vaginal area.
Diagnosis of Vaginismus
If you suspect you have vaginismus, it’s important to see a healthcare professional, typically a gynecologist or a sexual health specialist. The doctor will take a detailed medical history, including any psychological factors or past traumatic experiences, and may perform a pelvic exam to check for physical issues like infections or muscle tightness.
In some cases, additional tests, such as ultrasounds or MRIs, might be used to rule out other medical conditions. A diagnosis of vaginismus is typically made when no other medical explanation for the pain or inability to insert objects into the vagina can be found.
Treatment Options for Vaginismus
The good news is that vaginismus is treatable, and many women can overcome it with the right combination of approaches. Treatment plans often involve a mix of physical and psychological strategies, and what works will vary from person to person. Common treatment options include:
1. Pelvic Floor Therapy (Physical Therapy)
Pelvic floor therapy is often the first line of treatment. A trained physical therapist can help women learn to relax and control their pelvic floor muscles. This type of therapy may involve exercises to release tension in the vaginal muscles, as well as techniques to improve the strength and flexibility of the pelvic area.
2. Gradual Desensitization (Dilator Therapy)
Gradual desensitization involves the use of vaginal dilators of different sizes. A woman may start with the smallest dilator and gradually work her way up to larger sizes as she becomes more comfortable. This process allows the muscles to relax and helps the brain overcome any fear or anxiety related to penetration.
3. Cognitive Behavioral Therapy (CBT)
Cognitive Behavioral Therapy is a form of counseling that focuses on identifying and changing negative thought patterns. If vaginismus is rooted in anxiety, fear, or past trauma, CBT can be incredibly helpful in changing these thought patterns and addressing emotional barriers to sexual activity.
4. Sex Therapy
For couples experiencing vaginismus, sex therapy can be a valuable tool. A sex therapist helps both partners explore any emotional or relational factors that may be contributing to the problem. This therapy often involves communication exercises, relaxation techniques, and strategies to improve intimacy.
5. Botox Injections
In some cases, if other treatments have not been successful, doctors may recommend Botox injections to temporarily paralyze the vaginal muscles and allow them to relax. This can help break the cycle of muscle spasms and allow other treatments, like dilator therapy, to be more effective.
6. Medications
While medications are not typically the first treatment for vaginismus, certain medications may help manage pain or anxiety. This may include the use of local anesthetics (such as lidocaine) to numb the area or anti-anxiety medications for psychological relief.
Coping with the Emotional Impact of Vaginismus
Living with vaginismus can take a toll on a woman’s emotional health. It may lead to feelings of shame, frustration, isolation, and anxiety about relationships. It’s important to remember that vaginismus is a treatable condition, and seeking help is the first step toward overcoming it.
Here are a few tips for coping with the emotional impact of vaginismus:
- Communicate openly with your partner about the challenges you’re facing. Mutual support and understanding are crucial in navigating the emotional aspects of the condition.
- Practice self-compassion and remind yourself that vaginismus is not your fault. It’s a medical condition, and it doesn’t define your worth or ability to have a fulfilling sexual relationship.
- Seek support groups or counseling to connect with others who may be going through similar experiences.
Final Thoughts
Vaginismus is a common yet often misunderstood condition that can affect a woman’s sexual health and overall quality of life. It’s important to remember that it is treatable, and seeking professional help can lead to significant improvements. Whether through physical therapy, counseling, or medical treatments, many women find relief and are able to enjoy fulfilling sexual relationships once again.
If you suspect you have vaginismus, don’t hesitate to talk to your healthcare provider. With the right support, education, and treatment, vaginismus is a challenge that can be overcome.

Very good article – my compliments!
Dr Julia Reeve – Vaginismus Expert, Gynaecologist, Psychotherapist & Sexologist.
Very good article – my compliments!
Dr Julia Reeve – Vaginismus Expert, Gynaecologist, Psychotherapist & Sexologist.
thank you so much for your feedback.